Canada Life explains why the healthcare system is currently in "a paradox" and where plan sponsors should invest in wellbeing and prevention strategies

Despite surging investments in health and wellness, the overall health of Canadian workers is on a downward trend. And for Ilana Korble and Carolyn Chapman, health consultants at Canada Life, that contradiction reveals a bigger problem and a growing cost for plan sponsors.
“In spite of increasing spending, the health of Canadians is actually deteriorating,” Korble said at the Canadian Pension & Benefits Institute (CPBI) Forum in a seminar on Tuesday.
She emphasized that Canada’s healthcare system is currently in “a paradox” because while public and private spending on health and wellness has soared, nearly half of Canadians now have at least one chronic condition. Meanwhile, rates of obesity and type 2 diabetes have nearly doubled in the last 20 years.
“In 2023, over 30 per cent of Canadian adults were classified as obese. That increased from 21 per cent 20 years ago, and then from 9 per cent from 40 years ago and we know that obesity is a major risk factor for many diseases. Over approximately the last 20 years, the incidence of type two diabetes in Canada also increased,” she said, adding that 6 per cent of adult Canadians who live with pre-diabetic symptoms could end up living with diabetes.
“We have an opportunity here to mitigate that trajectory,” she added.
Korble also underscored how benefit plans are absorbing the shock as Canada Life has seen a continued increase in claims in their short-term and long-term disability block. And more of those claims involve poly-morbidities. Mental health, she added, is now linked to nearly 40 per cent of short-term disability claims.
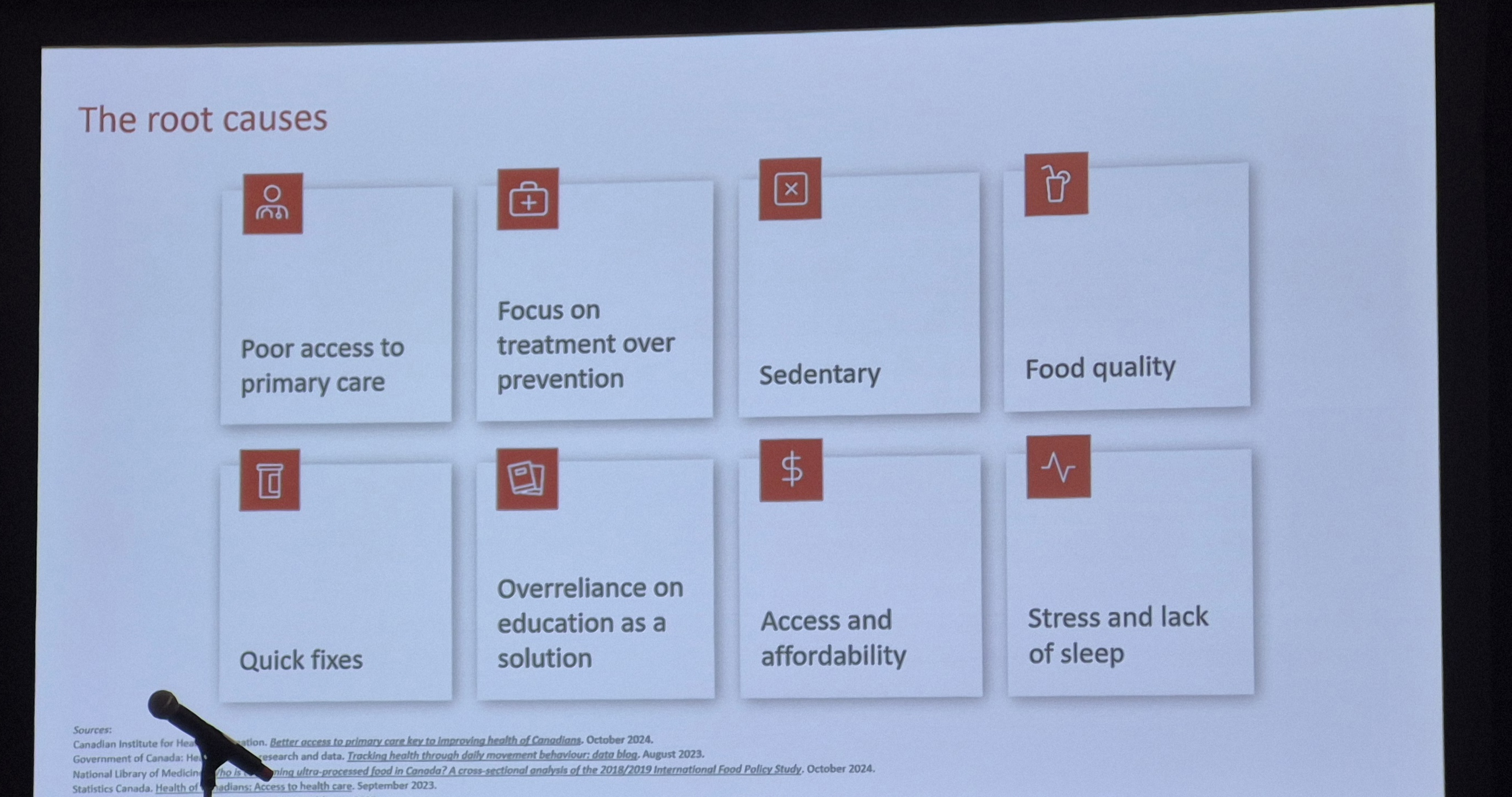
So, what’s driving the decline in health despite all this investment? Korble believes the healthcare system is focused heavily on treatment versus prevention as just 5 per cent of Canada’s healthcare spending went to prevention in 2023, she noted.
She likens the current system to a leaky bucket. The more money pumped in, whether through medications, wellness programs, or new technologies, the less return on investment sponsors are seeing. The bucket, she added, represents the healthcare system, and the water represents the spending.
“The holes really represent the underlying issues that we haven’t addressed,” she said, arguing that until those holes are patched, outcomes will continue to deteriorate regardless of input. “It's not just about medication, but it's about having that robust wellness strategy and program to keep Canadians in the Canadian workforce in that wellness space… The health of the workforce is not improving so are we investing in the right things? Are we missing the bigger picture when it comes to improving health and well being?”
Both Korble and Chapman see this failure to fix foundational issues as a warning sign for plan sponsors. The complexity of today’s benefit plans often masks a deeper problem because they’re not targeted, they’re not measurable, and often, they’re not personal.
“We tend to chase the next shiny thing,” Korble said, “but what we don’t often do well is maximize the value of what the program already has,” pointing to employee assistance programs (EAPs).
Additionally, Korble noted many members don’t recall what services exist or how to access them, especially if those benefits were only mentioned at onboarding.
“Targeted communication that personalizes the message becomes so important,” she said.
Chapman pointed to the need for ongoing engagement, not just one-time awareness campaigns, highlighting Carleton University’s Healthy Workplace strategy as a model of how sustained communication, internal partnerships, and tracking outcomes can drive change.
“They really leaned into their EAP, their insurer, and their people,” she explained, referencing how Carleton used lunchtime workshops, faculty expertise, and podcast content to connect with employees. The result led to a 131 per cent increase in program participation.
Chapman believes data plays a central role in transforming these strategies from hopeful ideas into practical tools. “If you’re not measuring and tracking, you’re pretty much guessing,” Chapman said, emphasizing that most employers know little more than a plan member’s name, age, and postal code.
“You have to go deeper than that,” she added. That includes understanding cultural and gender diversity, caregiving responsibilities, and financial pressure.
Korble added that economic strain is an often-overlooked driver of poor health. Gym memberships, healthy food and sleep routines become luxury items when plan members are struggling to pay their bills. In 2025, 42 per cent of Canadians cited money as their number one stressor, up from 38 per cent in 2021 during a pandemic, she said.
As for what plan sponsors should do, Chapman underscored that it starts with asking the right questions and more importantly, listening to the answers.
“Use surveys, utilization data, claim trends, health risk assessments,” she said. “You need all of it.”
She also emphasized the value of drug and paramedical data to understand plan member behaviour. For example, younger plan members are now spending far more on mental health services than older ones, and depression medications are top claims across every demographic.
That’s why Korble ultimately sees benefit programs as a critical touchpoint for prevention, if they’re designed with precision.
“Virtual care, for instance, can provide that quicker access,” she said, emphasizing that it’s not just about seeing a doctor. “It’s about getting the blood requisition or the referral before things escalate.”
But the responsibility doesn’t lie solely with employers. “We would argue that it’s not the role of the plan sponsor alone,” Korble said. “It’s a mutual responsibility. Both ember and sponsor. We all have a role to play in increasing health and staying healthy.”
Chapman acknowledged that plan sponsors need to encourage their members to take part in surveys, using benefits, and offering honest feedback. Because without that engagement, personalization efforts will fall short.
Ultimately, the pair agree that plan sponsors need to rethink chronic illness.
“The biggest piece is that it’s preventable,” Korble said, underscoring targeting modifiable risks like diet, activity, and sleep with tools that resonate and remove barriers.
“It’s not always about adding new programs,” she said. “It’s about making better use of what’s already there.”