Clear roles and data validation can increase efficiencies and help employers offer a competitive benefits plan to attract and retain top talent

Plan sponsors that adequately manage, administer, and promote their group benefit plans can create opportunities be leveraging governance and streamlining existing tools, says Normandin Beaudry. At a time when labour shortages are growing, it is important to have a group benefit plan that is competitive so it attracts talent, increases performance, and improves the employee experience.
Good tools free up time for HR departments so they can focus on value-added tasks rather than transactional ones, says Nathalie Lemieux, senior principal, group benefits with Normandin Beaudry, an actuarial and total rewards consulting services company. She says having efficient systems reduces the risk of errors associated with manual processes, such as premiums overpaid to insurance companies or employees not covered on time and having to provide proof of good health.
In-house systems have certain advantages for very large organizations. When a company needs to invest substantial sums to ensure the sustainability of these systems, it becomes crucial to seek guidance in selecting and implementing a system better suited to its needs. A good system can quickly improve employee autonomy by providing them with user-friendly and round-the-clock access to information.
For a company with many divisions, bringing in external specialists to assess its processes can be beneficial. They can make recommendations for simplifying and optimizing existing processes, while clarifying the roles and responsibilities of each stakeholder by using flow diagrams; this can greatly improve efficiency.
In addition, some non-value-added tasks can be outsourced to a third party, thus standardizing processing between divisions, freeing up internal resources and reducing the risks associated with employee turnover and errors due to inadequate documentation or training.
Assessing needs to reduce administration costs
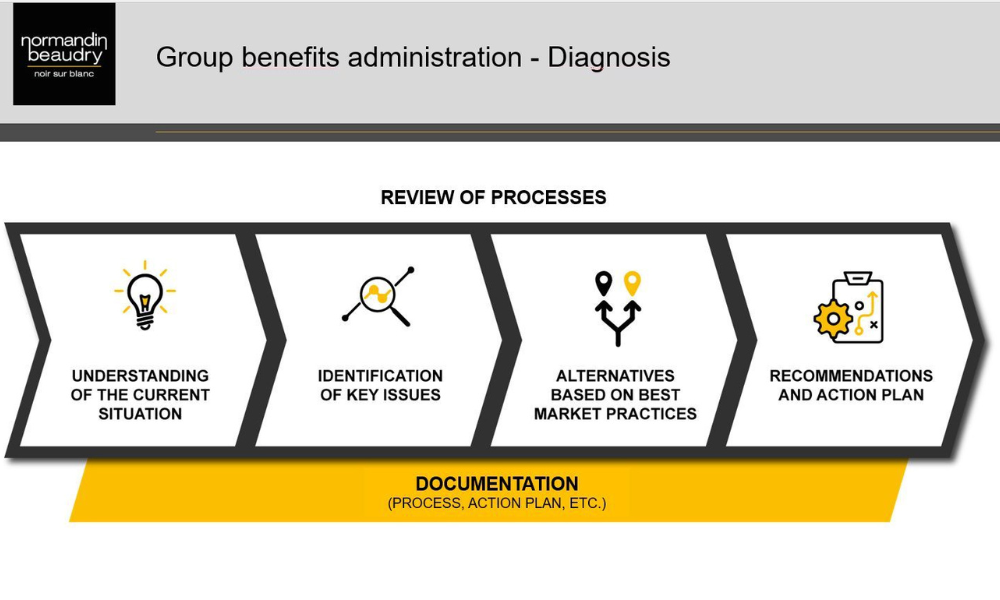
Companies considering changes or upgrades to their benefits administration need to assess their current systems and needs to see where they might make improvements or increase efficiencies, says Lemieux.
There are many ways to save on the administration of a group benefits plan. An organization whose administrative services costs are no longer sustainable can, for example, request a brief assessment of its needs to identify elements that were complicating the administration of their plan. Streamlining some of the plan’s parameters can result in substantial savings for the organization.
Lemieux says establishing a governance document is also important.
“Governance establishes and makes clear the roles and responsibilities for each stakeholder. This includes carriers and administrators. We often see that one division is not doing the same thing or is not applying the same rules as another division because there are no documents that clarify roles. There needs to be one place to put all the documentation together so that it's easy for everyone to find the information. If this is not available, the system will have a loss of efficiency.”
Data validation key to efficiency
Data validation is another key element of efficient systems.
“Data should be validated, but this can be difficult with all the different systems that are in place such as a payroll system, an HRIS system, and an administration system with another party. There are files that are provided to each of them to make sure that the data will flow. But, at some point, some data could be missed and it is only identified after the fact that some employees have not been terminated from the system, for example, and they're still paying a premium for those. We know that there are a lot of manual interventions done in the systems, and this could create errors.
“I usually recommend that my clients validate their data at least twice a year. They should be validating their data extract report files and compare them together. As well, if they know there are manual intervention processes, these should be validated and reviewed to avoid future issues. Fixing these mistakes down the road takes much more time and money than fixing them preventatively.
“Employers want to offer a group benefits plan that represents the culture and values of the company. The plan will demonstrate that the organization is taking care of their employees. By enhancing the administration and processes, the benefits plan will be a competitive advantage and the employer will be able to establish itself as an employer of choice.
“Employers must make sure the benefits plan is aligned with what their employees want and need. They need to offer tools, like mobile apps or virtual care, that are easy to use, well integrated with the plan, and provide a streamlined experience. Equipping the organization with the right tools and systems can help foster employee autonomy and grant them unrestricted access to information. If an employee has a child that is sick and their plan makes it easy to consult a doctor, that’s all an experience of working for that employer.”
For job seekers, group benefits are the second most important factor after salary. With the growing labour shortage, it is more important than ever to offer a group benefit plan that fosters talent retention and performance, while improving the employee experience.
Choosing smarter solutions can maximize the full potential of existing tools to better fit the employer and employee needs, all without significant new investments to optimize in-house tools or those offered by the insurance company or other third-party administrators.
There are solutions adapted to each organization’s specific needs based on existing plan features, interactions required between the various providers, and administrative practices specific to each organization.



